Two sets of financial accounting standards are generally accepted accounting principles (GAAP) and statutory accounting practices (SAP). One true statement about these financial accounting standards is that
The Titanium health plan's product has a unit price of $120 PMPM and a unit variable cost of $80 PMPM. Titanium has $100,000 in fixed costs per month. This information indicates that, for its product, Titanium's
The Arista Health Plan is evaluating the following four groups that have applied for group healthcare coverage:
With respect to the relative degree of risk to Arista represented by these four companies, the company that would most likely expose Arista to the lowest risk is the:
Geena Falk is eligible for both Medicare and Medicaid coverage. If Ms. Falk incurs a covered expense, then:
The Landau health plan will switch from using top-down budgeting to using bottom-up budgeting. One potential advantage to Landau of making this switch is that, compared to top-down budgeting, bottom-up budgeting is more likely to
With regard to the major risk factors associated with group underwriting, it can correctly be stated that, typically,
One law prohibits Dr. Laura Cole from making a referral to another provider entity for designated health services if Dr. Cole or one of her immediate family members has a financial relationship with the entity. This law is known as the
The Fiesta Health Plan prices its products in such a way that the rates for its products are reasonable, adequate, equitable, and competitive. Fiesta is using blended rating to calculate a premium rate for the Murdock Company, a large employer. Fiesta has assigned a credibility factor of 0.6 to Murdock. Fiesta has also determined that Murdock's manual rate is $200 PMPM and that Murdock's experience rate is $180 PMPM.
According to regulations, Fiesta's premium rates are reasonable if they
The sentence below contains two pairs of terms enclosed in parentheses.
Determine which term in each pair correctly completes the statement. Then select the answer choice containing the two terms that you have selected. In analyzing its financial data, a health plan would use (horizontal/common size financial statement) analysis to measure the numerical amount that corresponding items change from one financial statement to another over consecutive accounting periods, and the health plan would use (trend/vertical) analysis to show the relationship of each financial statement item to another financial statement item.
Under the doctrine of corporate negligence, a health plan and its physician administrators may be held directly liable to patients or providers for failing to investigate adequately the competence of healthcare providers whom it employs or with whom it contracts, particularly where the health plan actually provides healthcare services or restricts the patient's/enrollee's choice of physician.
The following statements are about pure risk and speculative risk—two kinds of risk that both businesses and individuals experience. Select the answer choice containing the correct statement.
Federal law addresses the relationship between Medicare- or Medicaid contracting health plans and providers who are at "substantial financial risk."
Under federal law, Medicare- or Medicaid-contracting health plans
This concept, which is an extension of the going-concern concept, holds that the value of an asset that a company reports in its accounting records should be the asset's historical cost, not its current market value. Although this concept offers objectivity and reliability, it may lack relevance, particularly for assets held for a long period of time.
From the following answer choices, choose the name of the accounting concept that matches the description.
The Caribou health plan is a for-profit organization. The financial statements that Caribou prepares include balance sheets, income statements, and cash flow statements. To prepare its cash flow statement, Caribou begins with the net income figure as reported on its income statement and then reconciles this amount to operating cash flows through a series of adjustments. Changes in Caribou's cash flow occur as a result of the health plan's operating activities, investing activities, and financing activities.
To prepare its cash flow statement, Caribou uses the direct method rather than the indirect method.
Several federal agencies establish rules and requirements that affect health plans. One of these agencies is the Department of Labor (DOL), which is primarily responsible for _________.
Experience rating and manual rating are two rating methods that the Cheshire health plan uses to determine its premium rates. One difference between these two methods is that, under experience rating, Cheshire
The following paragraph contains an incomplete statement. Select the answer choice containing the term that correctly completes the statement. Health plans face four contingency risks (C-risks): asset risk (C-1), pricing risk (C-2), interest-rate risk (C-3), and general management risk (C-4). Of these risks, ________________ is typically the most important risk that health plans face. This is true because a sizable portion of the total expenses and liabilities faced by a health plan come from contractual obligations to pay for future medical costs, and the exact amount of these costs is not known when the healthcare coverage is priced.
The Violin Company offers its employees a triple option of health plans: an HMO, an HMO with a point of service (POS) option, and an indemnity plan.
Premiums are lowest for the HMO option and highest for the indemnity plan. Violin employees who anticipate that they will be individual low utilizes of healthcare services are most likely to enroll in the
Advantages to a company that elects to self-fund and to administer all aspects of its healthcare benefit plan include:
The Swann Health Plan excludes mental health coverage from its basic health benefit plan. Coverage for mental health is provided by a specialty health plan called a managed behavioral health organization (MBHO). This arrangement recognizes the fact that distinct administrative and clinical expertise is required to effectively manage mental health services. This information indicates that Swann manages mental health services through the use of a:
The following information was presented on one of the financial statements prepared by the Rouge Health Plan as of December 31, 1998:
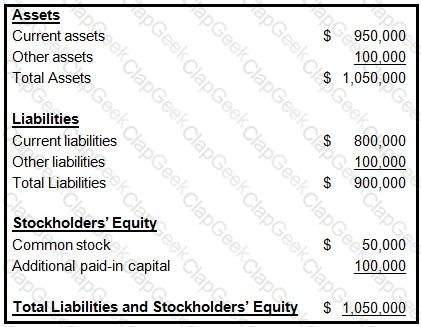
This type of financial statement is called:
Assume that the Lambda, Mesa, and Novella health plans are equal in every way except that the health plans have obtained equal amounts of net cash inflows from different sources, as shown below:
HealthPlan Source
LambdaFinancing activities
Mesa Investing activities
NovellaOperating activities
From the following answer choices, select the response which indicates the health plan that would most likely be the most attractive to a potential plan sponsor, to a potential creditor, and to a potential investor.
In order to show the efficiency of a health plan's managers in using the health plan's investments to earn a return for stockholders, a financial analyst most likely would use a type of profitability ratio known as
The Northwest Company offers its employees the option of choosing to receive their healthcare benefits from an HMO or from a traditional indemnity plan. The premiums for the HMO are lower than for the traditional indemnity plan. In this situation, it is correct to assume that:
1. Individual low utilizers are more likely to enroll in the traditional indemnity plan
2. Individual high utilizers are more likely to enroll in the HMO
In order to achieve its goal of improved customer service, the Evergreen Health Plan will add three new customer service representatives to its existing staff, install a new switching station, and install additional phone lines. In this situation, the cost that would be classified as a sunk cost, rather than a differential cost, is the expense associated with:
The following examples describe situations that expose an individual or a health plan to either pure risk or speculative risk:
Example 1 — A health plan invested in 1,000 shares of stock issued by a technology company.
Example 2 — An individual could contract a terminal illness.
Example 3 — A health plan purchased a new information system.
Example 4 — A health plan could be held liable for the negligent acts of an employee.
The examples that describe pure risk are
In order to determine a health plan's quick liquidity ratio, a financial analyst would divide the health plan's
The Fairway health plan is a for-profit health plan that issues stock. The following data was taken from Fairway's financial statements:
Current assets.....$5,000,000
Total assets.....6,000,000
Current liabilities.....2,500,000
Total liabilities.....3,600,000
Stockholders' equity.....2,400,000
Fairway's total revenues for the previous financial period were $7,200,000, and its net income for that period was $180,000.
From this data, Fairway can determine both its current ratio and its net working capital. Fairway would correctly determine that its
The Column health plan is in the process of developing a strategic plan.
The following statements are about this strategic plan. Three of the statements are true, and one statement is false. Select the answer choice containing the FALSE statement.


